This is a serious question. Do we as health care organizations, payors, health systems, providers – people – go far enough to reach the person we are serving and impact change right at their level? Do the existing person-centric efforts go far enough or is it just lip service to stay on top of the latest trends to meet consumer demand for a different experience?
How deeply do we know the people we are serving? As leaders in health care, we must be able to answer this question. Quadruple aim intentions are counting on us. And so are the American people.
2024 is expected to be the apex of boomer retirement causing a sharp increase in demand for senior health care services. And yet for this population, person-centered services have taken a back seat in an acute-care-first world. We’ve gotten senior care all wrong. We are great at solving disease and complex problems, but we’ve led the individual through a revolving door of reactionary, fragmented, and siloed services. And we are losing their greatest contributions to society – their spark.
I had the great opportunity to sit down with Dr. John Whyte, Chief Medical Officer for WebMD, to talk about how our industry has changed because of COVID. Let me be clear, COVID was only the accelerant. When the pandemic hit, it accelerated a firestorm already brewing and uncovered vulnerabilities within the health system in a way never seen before, especially for the senior population most impacted by COVID which largely played out in the home and community where gaps in access often occur. What we saw was just how inhumane health care can be and yet at the same time, how incredible the human spirit is within our communities.
If there is any silver lining to be had here, it’s that we had to pause, let the hospitals shift gears to focus on their core capabilities which are valued and needed, and allow innovations to take hold to meet people where they live – at home.
And now value-based payment mechanisms are finally catching on. We’re able to reap the value of the long-term relationships we are building with people to keep them well. No longer are those of us who are moving the center of health care home in a place where we prevent hospitalizations, create a lot of value, and yet don’t get paid for it. No longer are we in a place where technology is only about having data and metrics because it isn’t – you need the intelligence and the relationship.
All of these things have brought us to a crossroad that is quickly turning into a movement – will you choose wellness or more reactionary sick care?
To truly be person-centered, ‘whole person,’ or ‘person-centric,’ you remove the lens of episodic care. You talk to the person in your ‘care’ like a human. You understand what motivates them, spend a bit more time uncovering and discovering their purpose and passion. You build the relationships that matter with those you serve, know them like they want to know you. You uncover that Betty fell and broke her hip not because of ‘normal aging’ but because she lost her husband and was grieving. She like any spouse of any age was navigating her new normal and we need to be by her side along that journey healing both her heart and her hip. Even better, you could have been involved sooner and prevented her fall – imagine what that would have saved?
You also uncover that Jeff lives in senior living, volunteers, plays the guitar, and is an athlete. How do we bridge opportunities to keep him doing what he loves, right where he lives? You create TRYathalons and nurture the competitive spirit because if you don’t, he will lose that purpose where isolation and loneliness creep in. And when Tammy’s mother could have continued spiraling on the roller coaster of health care crises, they took a chance and chose life by engaging in a trusted health care professional who truly understood both. An integrated team that valued their life goals and helped them achieve that experience.
All of this should be the experience you get when you have health insurance and receive health services. Using it to not just process claims data, or provide another script, ‘ologist,’ unnecessary x-rays or blood work that pose significant hurdles to a senior.
Putting the humanity into health care is all about connecting people to more life, more magnificence, more community, more home, more systems of excellence that are listening to what seniors and their family caregivers want.
We can do better. When we do, we see humanity find its way back in.
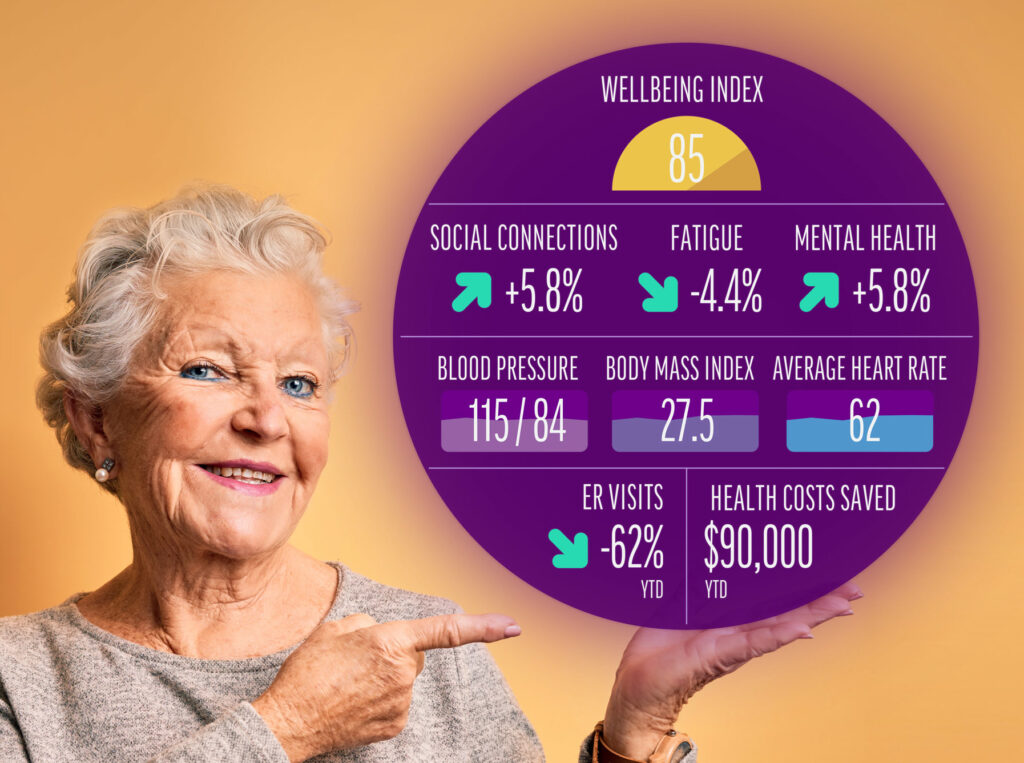
In all of these situations, when we focus on the person, on providing value and not volume, we improve the complete experience for all the stakeholders; cost is reduced, the experience for both the senior and the employees working with them are improved, and we start to see improved health of our collective populations. That is the intent of quadruple aim. Just one senior who has a better experience creates a ripple effect that can be a powerful catalyst for change. This isn’t lip service – at Lifespark, we have data, real raw data, that proves it. And we have our people. Their experience provides a snapshot of possibility of what every American can have as they age.
The Lifespark approach is a “human-to-human” delivery model that uses a high- tech-high touch approach to better understand the whole person health needs. This becomes the foundation for less friction in the system, reduced cost and better outcomes. More humanity in the delivery system will also usher in a shift from anti-aging to positive-aging thinking and approach. We know (thanks to science and our clinicians) that this “sparked” positive-aging mindset (vs an anti-aging mindset) helps us live longer, better.
To bring humanity back we must partner – isolation is fatal. We are proud to connect with bold visionaries, nurses, physicians, caregivers, payors, health systems, providers, thought leaders, and many others who believe humanity is sacred. Who realize that focusing on humanity is actually good for our bottom line. Kind of like aging magnificently is a rallying cry, restoring humanity with the center of health care in the home is the future. Truly investing in those buzzwords is something we must do.
But I’m curious, what do you think? Have we lost the humanity in health care? Let’s open the dialogue and watch the innovation and spark fly.
Joel Theisen RN, BSN is founder and CEO of Lifespark. A fierce competitor in both his professional and personal life, Joel is a seasoned Chief Executive with 30+ years, in long-term, home, and community-based services and an inspiring, and driven culture builder as well as a creative business partner. Visit our partner page to help us change the age-old story.


