Read time: 2 minutes
Back in 2021, while Bonnie was at the hospital visiting her husband, Bill, she noticed a Lifespark brochure on his nightstand. “I took one look at it and thought, ‘I’ve been a registered nurse for almost 70 years and my daughter, who lives with us, is also a nurse, so why would we need in-home nursing? We’re nurses,’” Bonnie said.
Since retiring nearly 20 years ago, Bonnie had been caring for her husband to help him manage his heart failure, diabetes, and chronic obstructive pulmonary disease (COPD). But by 2022, Bill’s health was in a steep decline. “We went back to the hospital many, many times, always waiting for hours in the waiting room and never seeing the same doctor twice,” she said.
After yet another hospitalization, Bonnie remembered the Lifespark brochure. “It dawned on me one day that these nurses could be supportive to me, like colleagues in a way, so we decided to give it a try,” she said.
Guidance and support
With Bonnie’s help, Bill enrolled in Lifespark COMPLETE, giving him access to a dedicated advisor and an in-home medical expert at no additional cost to him, thanks to a partnership between Lifespark and UCare, Bill’s Medicare plan.
He started working with a Life Manager but wanted to keep seeing his primary care provider. Bonnie was managing Bill’s medications and bandaging his leg wounds, but between his frequent falls and difficulty with stairs, she didn’t feel safe being his only support. That’s when Katelin Super, NP, Lifespark Nurse Practitioner, got involved.
Strength, safety, and independence
“Bill had a number of serious medical issues that required frequent monitoring, but it was becoming too difficult for him to get to his clinic,” Katelin said. “I took on the role of primary care provider but communicated regularly with his doctor who had a good relationship with Bill.” She checked his vitals, coordinated in-home labs for blood draws and lung X-rays, and followed up with his specialists.
After his most recent hospitalization, he had been referred to an acute rehabilitation facility for physical therapy (PT), occupational therapy (OT), and skilled nursing. But as Bonnie explained, “Bill hated the idea of going to a TCU [Transitional Care Unit] because he’d had such a terrible experience at the last one. He just wanted to come home to hang out in his mancave and listen to country music as loud as he wanted.”
To help Bill rebuild his strength at home, Katelin coordinated with Lifespark Skilled Home Health to bring in PT, OT, and special medical equipment. Bill was learning to walk with a cane, but as his condition declined, he progressed to a walker. The OT team rearranged furniture to create safe pathways and taught him how to navigate his environment while managing the oxygen tubing.
It was also important to Bill that he maintain his independence with his activities of daily living, particularly showering and dressing. To do that, OT brought in equipment and trained him how to use it. Stairs were still a challenge, so Bonnie gave him a whistle to use when he needed help.
Controversial topic
Despite the team’s best efforts to create a safe environment, Bill sustained several painful falls. Katelin ordered in-home X-rays to evaluate for injuries, but the emergency room visits and hospitalizations continued.
“I’ve known Bill for over two years, and it’s always been his wish to stay in his house until the end of his life,” she said. “Still, every time he was hospitalized, the question would come up whether it was appropriate for him to come home or if he needed to be transferred to a higher level of care.”
As Bill’s caregiver and a seasoned nurse with decades of long-term care experience, Bonnie was keenly aware of her husband’s decline. “Every hospital stay left him more disabled, but I knew he didn’t want to go to a nursing home,” she said. “I brought up the idea of hospice which created a lot of controversy in our family, mostly because they thought hospice is a death sentence, but that’s just not true.”
Bill was also against it, but after talking with his Life Manager, Holly Gustav, RN, who joined the team in November, he warmed up to the idea. “Once we explained that hospice would bring in extra services that would help him meet his goal of living at home, he was on board,” Holly said.
Since enrolling in Lifespark Hospice, Bill hasn’t returned to the hospital, she said, adding that Bonnie knows what signs and symptoms to watch for and when to call for a medication change.
The gifts of hospice
Bill is taking full advantage of what hospice has to offer, Holly said. “He really enjoys getting massages, spending time with the Lifespark chaplain, and singing along with the music therapist,” she said. “These visits truly enrich his life.”
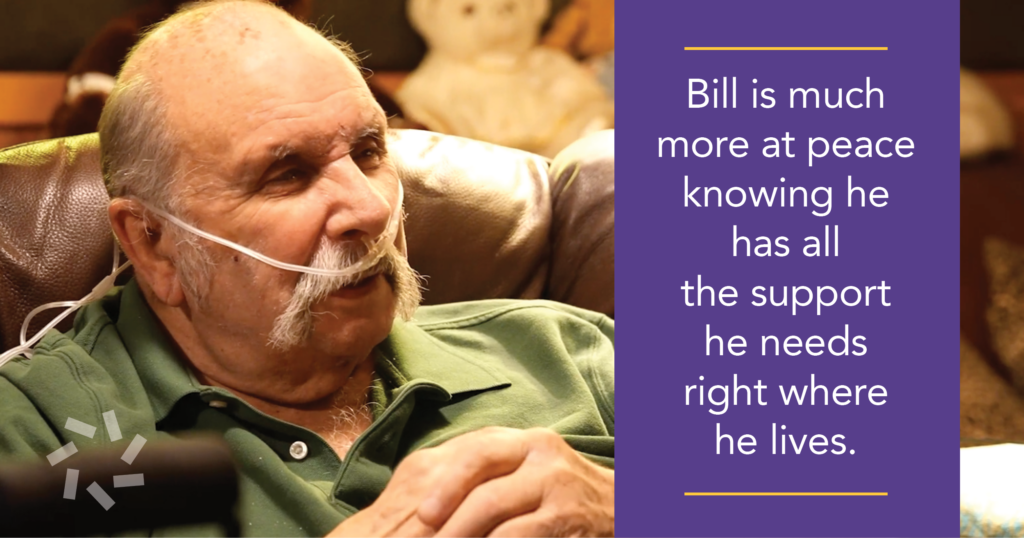
According to Katelin, Bill is much more at peace with his health conditions, knowing he has all the support he needs right where he lives. “Now that he’s engaged with the hospice team and receiving these services, he understands that this is about keeping him comfortable,” she said.
Bonnie is still his primary caregiver, but hospice has given her an added layer of support, as well. “I was really sad one day, so I called Lifespark and they came over to support me,” she said. “These people give their best every time, but they’re not just professionals—they’ve become friends to us. We couldn’t be happier.”
To learn how Lifespark can help you or a loved one live life on your terms, call 952-345-8770 or visit Lifespark.com.